10
Impact Factor
ISSN: 1449-2288
Int J Biol Sci 2023; 19(13):4157-4165. doi:10.7150/ijbs.86492 This issue Cite
Review
The PTGS2/COX2-PGE2 signaling cascade in inflammation: Pro or anti? A case study with type 1 diabetes mellitus
1. Andalusian Center of Molecular Biology and Regenerative Medicine CABIMER, Junta de Andalucia-University of Pablo de Olavide-University of Seville-CSIC, Seville, Spain.
2. Centro de Investigacion Biomedica en Red de Diabetes y Enfermedades Metabolicas Asociadas (CIBERDEM), Madrid, Spain.
Abstract
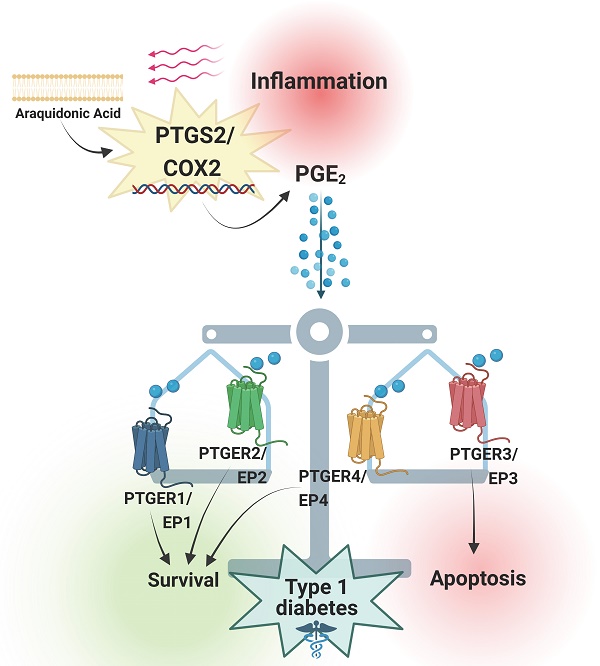
Prostaglandins are lipid mediators involved in physiological processes, such as constriction or dilation of blood vessels, but also pathophysiological processes, which include inflammation, pain and fever. They are produced by almost all cell types in the organism by activation of Prostaglandin endoperoxide synthases/Cyclooxygenases. The inducible Prostaglandin Endoperoxide Synthase 2/Cyclooxygenase 2 (PTGS2/COX2) plays an important role in pathologies associated with inflammatory signaling. The main product derived from PTGS2/COX2 expression and activation is Prostaglandin E2 (PGE2), which promotes a wide variety of tissue-specific effects, pending environmental inputs. One of the major sources of PGE2 are infiltrating inflammatory cells - the production of this molecule increases drastically in damaged tissues. Immune infiltration is a hallmark of type 1 diabetes mellitus, a multifactorial disease that leads to autoimmune-mediated pancreatic beta cell destruction. Controversial effects for the PTGS2/COX2-PGE2 signaling cascade in pancreatic islet cells subjected to diabetogenic conditions have been reported, allocating PGE2 as both, cause and consequence of inflammation. Herein, we review the main effects of this molecular pathway in a tissue-specific manner, with a special emphasis on beta cell mass protection/destruction and its potential role in the prevention or development of T1DM. We also discuss strategies to target this pathway for future therapies.
Keywords: Beta cells, Cyclooxygenases, Inflammation, Pancreatic Islets, Prostaglandin, Type 1 Diabetes Mellitus

 Global reach, higher impact
Global reach, higher impact