Impact Factor
ISSN: 1449-2288
Int J Biol Sci 2011; 7(2):138-146. doi:10.7150/ijbs.7.138 This issue Cite
Research Paper
Recurring Measles Epidemic in Vietnam 2005-2009: Implication for Strengthened Control Strategies
1. Department of Eco-epidemiology, Institute of Tropical Medicine Nagasaki University, 1-12-4 Sakamoto, Nagasaki 852-8523, Japan.
2. Department of Vector Ecology and Environment, Institute of Tropical Medicine Nagasaki University, 1-12-4 Sakamoto, Nagasaki 852-8523, Japan.
3. Department of Animal and Environmental Biology, Delta State University, Abraka, Nigeria.
4. Department of Occupation, Nha Trang Pasteur Institute, Khanh Hoa, Vietnam.
Received 2010-9-8; Accepted 2011-1-20; Published 2011-1-27
Abstract
Background: Measles remains a serious vaccine preventable cause of mortality in developing nations. Vietnam is aiming to achieve the level of immunity required to eliminate measles by maintaining a high coverage of routine first vaccinations in infants, routine second vaccinations at school entry and supplementary local campaigns in high-risk areas. Regular outbreaks of measles are reported, during 2005-2009.
Methods: National measles case-based surveillance data collected during 2005-June 2009 was analyzed to assess the epidemiological trend and risk factors associated with measles outbreak in Vietnam.
Results: Of the 36,282 measles suspected cases reported nationwide, only 7,086 cases were confirmed through laboratory examination. Although cyclical outbreaks occurred between 2005 and 2009, there was no definite trend in measles outbreaks during these periods. Overall, 2438 of measles confirmed cases were among children ≤5 years and 3068 cases were among people ≥16 years. The distribution with respect to gender skewed towards male (3667 cases) significant difference was not observed (P= 0.1693). Unsurprisingly, 4493 of the confirmed cases had no history of vaccination (X2 <0.01). The northern and highland regions were identified as the main endemic foci and the spatial distribution changed with time. The occurrence of cases, in a considerable proportion of vaccinated population, is not only a reflection of the high vaccination coverage in Vietnam but also portrays a possibility of less than 100% vaccine efficacy. More so, in order to prevent measles in adults, high-risk groups must be identified and catch-up for selected groups selected.
Conclusions: This study therefore reinforces the need for continued improvement of surveillance system and to probe into the possible role of changes in age-distribution of cases if the effective control of measles is to be achieved.
Keywords: Epidemiology, Measles, Outbreak, Vietnam
INTRODUCTION
Measles is an acute, highly communicable viral disease spread by respiratory secretions that may lead to serious complications such as diarrhea, otitis media, pneumonia or encephalitis [1]. Measles remains endemic wherever vaccination coverage is low and is one of the leading causes of vaccine preventable death in children worldwide [2]. Globally, the death rates from measles have declined sharply in the past decades, largely as a result of intensive vaccination efforts [3, 4]. Efforts to prevent measles deaths have aligned around the United Nations' Millennium Development Goals (MDGs), which identify childhood mortality reduction as a key priority [5]. Measles Contained Vaccine (MCV) vaccination programs form a cornerstone of these efforts with ambitious targets, including universal childhood measles vaccination and 90% reductions in measles deaths from year 2000 levels (733,000 worldwide) and in 2008, there were an estimated 164,000 measles deaths, a 78% reduction compared to mortality in 2000 [5,6].
In Viet-Nam, there has been substantial progress in controlling measles as evident by the adoption of the regional goal set by the WHO, Western Pacific region to eliminate measles, which was defined as terminating the circulation of domestic strain in the region by 2012 [7], yet sporadic epidemic do occur. This vividly shows the limitation of a single-dose approach in interrupting domestic circulation of the measles virus [8], to curtail this limitation; a nationwide mass immunization campaign was conducted mainly to provide a second dose vaccine to children aged 9 months to 9 years. As a consequence of the 2002 and 2003 nationwide campaign, measles confirmed cases were clearly suppressed in 2004. However, throughout 2005 and 2006 resurgence of measles epidemic occurred [9]. Here, we describe the trend in the epidemiology of measles in Vietnam during 2005-2009 with a view to identify the associated risk factors and to proffer viable solutions to strengthen the prevention and control of measles in Vietnam more effectively.
METHODS
Study Area
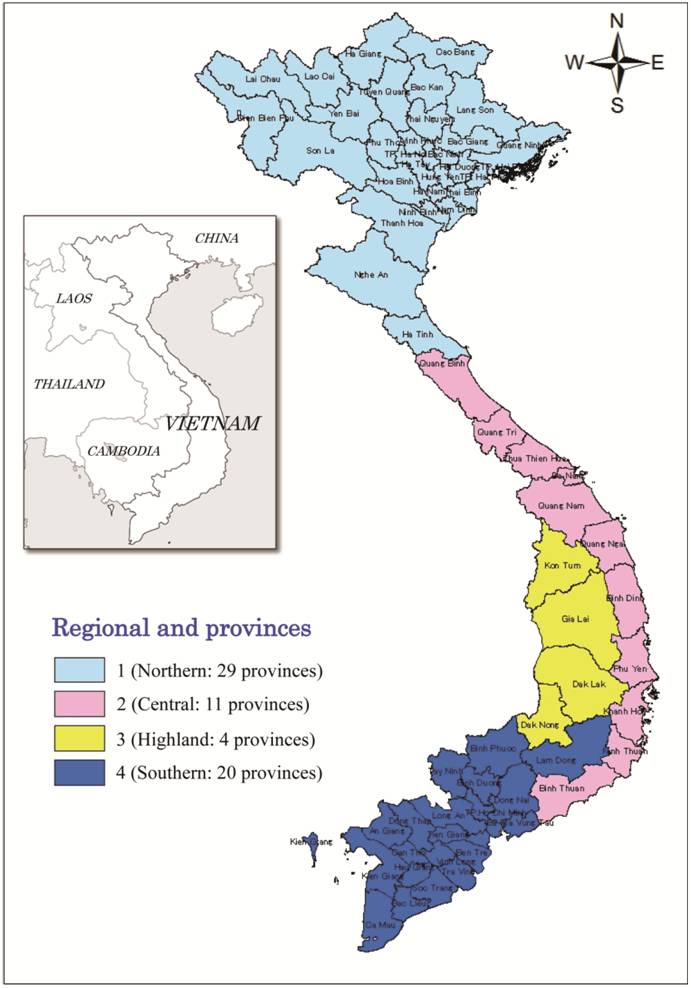
Vietnam is the largest and most populous of the 3 Indochinese countries and is located along the East Coast of Indochina and borders on Cambodia and Laos in the West and the Peoples Republic of China in the North. Based on geographical features and climate, Vietnam is divided into four regions (see fig 1). Although, the country is located in the tropics, the climate is tropical only in the central and southern Vietnam, with warm and humid weather all year round (22-350C). In the north, there is a distinct winter season due to cold inland winds, usually; the winter is also the dry season for the entire country, but the rains are highly unpredictable owing to the influence of several monsoons. Vietnam covers a total land area of 329314km2 with a population of approximately 88.6 million and a population density of 252 persons per km2 [10].
Data source and analysis
In this study, measles cases reported within the Vietnam measles surveillance system between 2005 and 2009 were investigated. Physicians were required to report all suspected measles cases and to obtain samples for confirmatory IgM testing at the national measles laboratories at the National Institute of Hygiene and Epidemiology in Hanoi or the Ho Chi Minh City Pasteur Institute in Ho Chi Minh City. Epidemiologic variables such as year, age, sex, vaccination status and province of resident were collected through case reporting forms filled by the physicians and vaccination status was a yes/no response previously vaccinated based on patient/parents recall and unknown vaccination status was excluded. Suspected cases in which laboratory test results were negative were discarded as non-measles thus only confirmed measles cases were used.
National measles surveillance data for Vietnam from 2005 through June 2009 wasanalyzed. The surveillance data set was originally maintained using Microsoft Access software (Microsoft Corp., Redmond WA, United States of America). Chi square test was used to determine significant difference in vaccination status as well as the gender related cases. Data was analyzed using SPSS 10.0J (SPSS Inc., Chicago IL, USA).
RESULTS
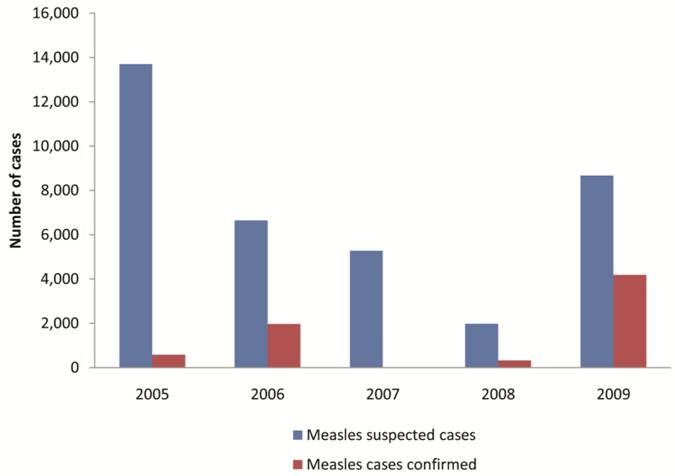
Of the 2005-2009 national measles surveillance data for Vietnam reviewed, 36,282 measles suspected cases were reported nationwide during these periods; only 7,086 cases were confirmed after proper laboratory examination. Although, cyclical outbreaks of measles occurred between 2005 and 2009, the cases showed no fixed trend. The number of confirmed cases increased from 581 in 2005 to 1975 cases in 2006 thereafter a sharp decrease to 17 cases in 2007. However, a resurgence 325 measles confirmed cases was observed in 2008, this outbreak increased progressively into 2009 with a total of 4188 confirmed cases (Figure 2).
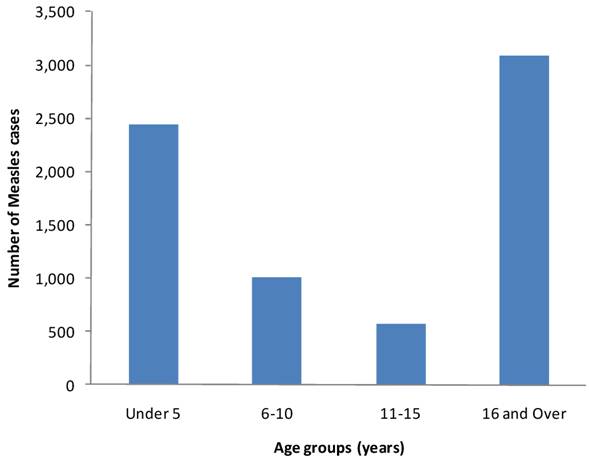
Data on figure 3 depicts the number of confirmed measles cases distribution by age groups. The distribution of cases in increasing order are 567, 1013, 2438 and 3068 for age groups 11-15, 6-10, ≤5 and ≥16 years respectively. Figure 3 further reveals that the peak age distribution has skewed from preschool children to people over 16 years.
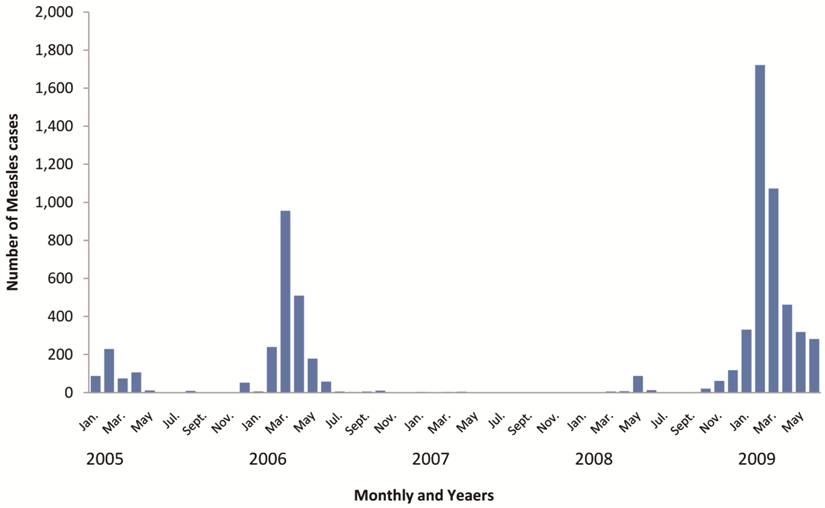
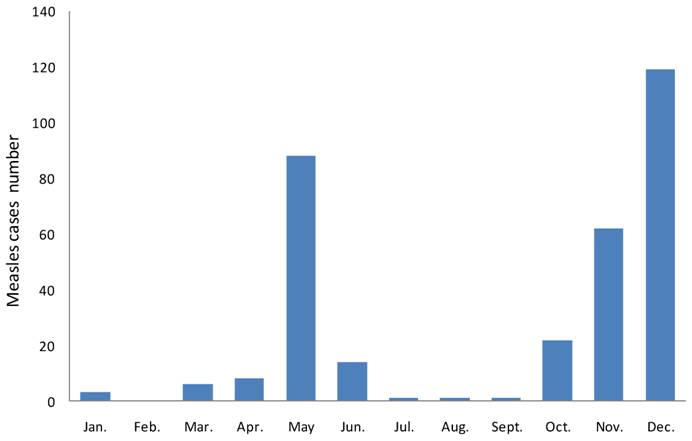
From January 2005 through June 2009, it was apparent that measles confirmed cases occur all year round though, outbreak starts in December and extend to May or June of the following year with peak in February and March (Figure 4). In 2008 two epidemics occurred, first in May and peaked in June while the second epidemic started in October and progressively increased (Figure 5).
Vietnam region area and provinces map- (Map of study area)
Measles distribution in Vietnam from 2005-2009
Pooled confirmed measles cases and percent distribution by age groups from 2005- 2009
Measles cases distribution by months and years from 2005-2009
Monthly measles cases and percent distribution for year 2008
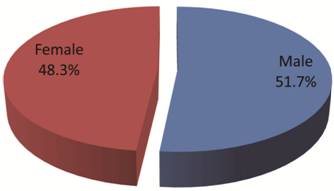
The distribution of confirmed measles cases with respect to gender is shown in Figure 6. Although, male had a higher cases (3667) than female (3419) chi square analysis showed no significant difference (P=0.1693).
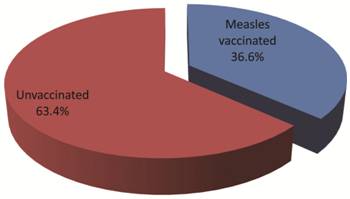
Data on figure 7 presents measles vaccination status of the 7,086 confirmed cases. Interestingly, 4493 of the subjects have no history of vaccination while 2593 were vaccinated (X2 < 0.01).
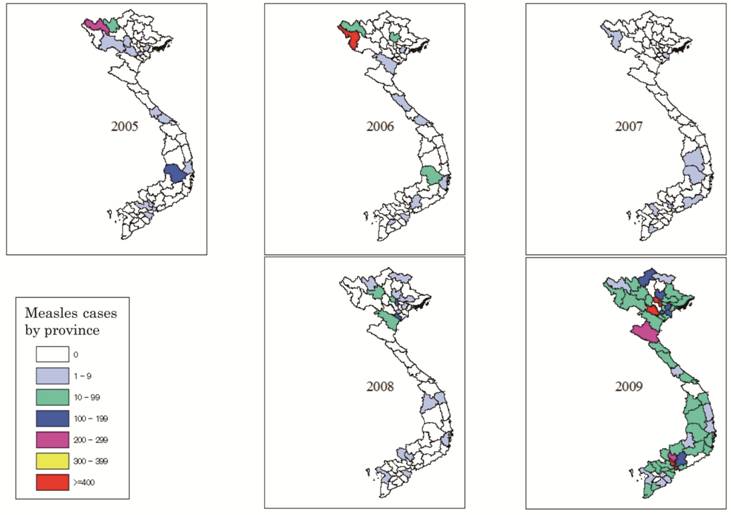
The spatial distribution map of measles from 2005 through 2009 reveals that measles epidemic occurred at different places with varied rates and a series of foci shifting in time and in space (Figure 8). The epidemic mostly occurred in the Northern and highland provinces while in 2009 it spread across the entire country.
Table 1 shows that the Northern region of Vietnam consistently maintained a high level of confirmed measles cases from 2005-2009. More so, Table 1 further reveals that the number of confirmed cases rose from 581 in 2005 to 1975 in 2006 while between 2008 and 2009 the figure rose from 325 cases to 4188 cases.
Pooled measles cases distribution by genders from 2005-2009
Measles vaccination status
Geographical distribution map of confirmed measles cases from 2005-2009
Confirmed regional measles case distribution from 2005-2009
| Region | Number and percentage of yearly confirmed Measles cases | |||||
|---|---|---|---|---|---|---|
| 2005 | 2006 | 2007 | 2008 | 2009 | Total | |
| Northern | 390(67.1) | 1917(97.1) | 2(11.8) | 314(96.6) | 2,781(66.4) | 5404(76.3) |
| Center | 5(0.9) | 4(0.2) | 1(5.9) | 5(1.5) | 127(3.0) | 142(2.0) |
| Highland | 181(31.2) | 48(2.4) | 6(35.3) | 1(0.3) | 126(3.0) | 362(5.1) |
| Southern | 5(0.9) | 6(0.3) | 8(47.1) | 5(1.5) | 1,154(27.6) | 1,178(16.6) |
| Total | 581(8.2) | 1,975(27.9) | 17(0.2) | 325(4.6) | 4,188(59.1) | 7,086(100.0) |
DISCUSSSION AND CONCLUSIONS
With the increasing vaccination coverage resulting from compulsory measles vaccination in 1985 as well as the 2002-2003 nationwide immunization campaign, the incidence of measles in Vietnam was significantly reduced. However, resurgences occurred in 2005 and 2008. The rapid resurgence in 2005 was implicated for lack of a swift introduction of a follow-up second immunization as routine second close immunization at school entry only started in after 2006 [9]. More so, the resurgence in 2008 could possibly be attributed to an accumulation of susceptible (non immune persons) to a critical threshold level. This observation is not only similar to the experience in other parts of developing countries, where campaigns among children under 5 years had a limited and transient impact [11, 12], but also further re-affirmed the reports of Duclos et al [13] and Ong et al [14] that the strategies that rely on administration of a single dose of measles vaccine are inadequate for the interruption of measles transmission.
Although, measles has traditionally been a disease affecting young children, especially those under 5 years, observation on the age group distribution depicts a shift in the age group of confirmed measles cases. 2438 cases were less than 5 years, this finding concurs with reports elsewhere for other countries [14-16]. However, the tremendously high number of cases (3068) occurring in persons over 16 years reconfirms that measles incidence in many countries may be explained by the changing epidemiology of measles following vaccination as predicted in mathematical models [17]. Our observation on the high proportion of measles cases in people over 16 years is in consonance with previous reports that pointed out an age shift in measles incidence to older susceptible [9, 12, 13, 18, 19]. In India, Kadri et al 2008 [19] reported that there is now a changing pattern in age affliction of measles; it is shifting towards the adult age groups. Their data shows an upward age shift in measles cases 55.6% of cases occurred beyond the 5th year of age, and as many as 20.88% cases were adults (>18 yrs age). Similarly, Murakami et al 2008 [9] observed that the national median age for measles cases in Vietnam shifted from 8-11 years after measles vaccination campaign. This shift in measles infection in adults is quite disturbing as it has serious consequences for children. First infected adults may not be able to work as well as caring for their children for some days. Secondly, infected adults could transmit measles virus to susceptible children. Third, susceptible mothers cannot confer protective anti-measles virus antibodies to newborn children, thus leaving them vulnerable to possible measles infection from their parents, sibling or other close contacts [20].
The measles control strategy implemented in Vietnam from 2002-2003, with mass immunization campaigns yielded considerable results. However, the impact was short lived as measles outbreak was detected as early as 2005 and in 2006, there was a larger resurgence of measles involving 1975 confirmed cases. A possible resurgence of measles in Vietnam during 2005-2006 is that older children remained vulnerable because the age group targeted for vaccination was narrower (9 months to 9 years) than recommend (9 month to 14 years) [21]. Throughout 2005 and 2006, the main focus of the resurgence was in the territory comprised by the former Lai Chau Province.
In the later part of 2006, the country introduced the second routine immunization dose given at school entry with coverage greater than 98%. This resulted to the suppression of measles from 1975 confirmed cases in 2006 to only 17 confirmed cases in 2007, thus confirming the reports of Adodool-Karim et al [22] that mass measles campaigns in partially immunized communities are expected to reduce measles incidence and shift the age distribution of cases to older children. The impact of the campaigns lasted only a few months and was followed by a rapid resurgence in measles cases in 2008, suggesting a sudden and explosive reintroduction of measles virus into the country. This is not different from the experience in other developing countries, where campaign had a limited and transient impact [11]. The resurgence in measles epidemic in 2008 progressively increased and peak in May (1920 cases). Although, the reported cases gradually decreased after September, the epidemic recurred in October of same year and produced a second higher peak of 2593 confirmed cases in December.
Vietnam has the advantage that coverage of routine first dose of measles vaccination is quite high: 98% and 94% in the north and south respectively, and in 2006, second routine immunization dose was introduced in 43 out of 64 provinces with coverage of 98% [9]. 2593 of the affected measles case had history of immunization. In spite of the reported high vaccination coverage, results from this study indicate that 4493 of the confirmed cases had no vaccination history thus confirming the suspicion of Murakami et al [9], that the immunization campaign may have been compromised locally. Furthermore, the unvaccinated subjects may have added to the accumulation of susceptible person that provide enough hosts to sustain and promote chains of measles virus transmission.
Measles epidemics in Vietnam from 2005-2009 were consistently higher in the northern and highland provinces suggesting that these areas remain endemic foci areas. This supports the observation of Murakami et al [9], who reported rapid resurgence of measles in the northern part of Vietnam and attributed this to the vulnerability of older children because of the age group targeted for vaccination was narrow.
Local measles outbreaks were detected as early as 2005 in the Lai Chau province and in Lao Cai province, both in the north-western mountainous region, despite the immunization campaign. This epidemic transcend into a large resurgence of measles involving 1917 confirmed cases. These Northern provinces are bordered by China and Laos suggesting an extensive impact of measles virus importation as border areas may be particularly vulnerable to importation of measles or other disease due to increased migration of people from neighboring countries.
Despite the widespread use of measles vaccine in the republic of Vietnam, secular trends and seasonal outbreaks of measles continues to occur. Several outbreaks have occurred in highly vaccinated population groups and many of these cases have been previously vaccinated.
This study depicts that the most common age groups affected during these periods 2005-2009 are ≤ 5 and ≥ 16 years respectively. To prevent future outbreaks, surveillance should be enhanced to achieve complete coverage as well as consideration of older age group to avoid accumulation of susceptible persons. In addition, measles “catch-up” mass immunization campaign should be conducted to interrupt chains of transmission and prevent outbreaks. Furthermore, in an area such as Vietnam where measles is endemic, the duration of impact of campaigns does not exceed two years, even in the best circumstances of high routine and campaign coverage, therefore, efforts should be geared to have follow-up campaigns 2-3 years later to reinforce the impact of mass campaigns. If Vietnam is aiming to achieve the level of immunity required to eliminate measles, it is therefore recommended that:
- Steps to prevent measles in adults should be highly considered, and this should include strict compliance to both first and second dose immunization among others as well as a wider age group campaign.
- Border areas of Vietnam may be vulnerable to importation of measles due to high migration of people thus ensuring high levels of immunological protection among residents of border areas, and by establishing sensitive and timely disease surveillance, as well as the need to investigate the dynamics of measles transmission should be a public health priority.
- Strengthening out of routine vaccination should be the cornerstone of measles control to achieve >90% coverage and it could be achieve by identifying population without access to routine vaccination and providing sustainable outreach services, coupled with adequate epidemiologic survey.
Acknowledgements
We would like to thank all public health professionals, primary health care professionals and clinicians for their collaboration and assistance in compiling the data. Our kind appreciation to the three anonymous reviewers for their noble comments that substantially strengthened this paper.
AUTHOR CONTRIBUTIONS
HTT conceived, designed the study, collected, analyzed the data and made the first draft in theses form. JCN wrote the paper and contributed to data interpretation. KG oversees the data analysis and interpretation and critical review of the manuscript for intellectual content. All authors read and approved the final manuscript.
COMPETING INTERESTS
The authors declare that they have no competing interests.
References
1. Heymann DL. Control of Communicable Diseases Manual 19th Edn. Washington DC: American Public Health Association. 2008
2. Martin N, Foxwell AR. Measles status in Australia, and outbreaks in the first quarter of 2009. Commun Dis Intell. 2009;33(2):255-231
3. Wolfson LJ, Strebel PM, Gacic-Dobo M, Hoekstra EJ, McFarland JW, Hersh BS. Has the 2005 measles mortality reduction goal been achieved? A natural history modelling study. Lancet. 2007;369:191-200
4. Wolfson LJ, Grais RF, Luquero FJ, Birmingham ME, Strebel PM. Estimates of measles case fatality ratios: a comprehensive review of community-based studies. Int J Epidemiology. 2009;38:192-205
5. Goldhaber-Fiebert JD, Lipsitch M, Mahal A, Zaslavsky AM, Salomon JA. Quantifying Child mortality reductions related to measles vaccination. PLoS ONE. 2010;5(11):e13842
6. CDC. Global Measles Mortality, 2000-2008. Morbidity and Mortality Weekly Report (MMWR). 2009;58(47):1321-1326
7. World Health Organization. Resolution number WPR/RC54.R3 (Expanded Programme on Immunization: measles and hepatitis B). Regional Office for the Western Pacific; 2003.
8. McFarland JW, Mansoor OD, Yang B. Accelerated measles control in the Western Pacific Region. J Infect Dis. 2003;187(1):246-241
9. Murakami H, Nguyen VC, Hong VT, Tsukamoto K, Do SH. Epidemiological impact of a nationwide measles immunization campaign in Vietnam: a critical review. Bulletin of the World Health Organization. 2008;86(12):948-955
10. Geography and climate. SADEC. http://www.sadec.com/Profile/viet05.html
11. Chen RT, Weierbach R, Bisoffi Z, Cutts TF, Rhodes P, Ramaroson S, Ntembagara C, Bizimana F. A 'post-honeymoon period' measles outbreak in Muyinga sector, Burundi, Burundi. Int J Epidemiol. 1994;23:185-193
12. Nanyunja M, Lewis RF, Makumbi I, Seruyange R, Kabwongera E, Mugyenyi P, Talisuna A. Impact of mass measles campaigns among children less than 5 years old in Uganda. J Infect Dis. 2003;187(1):63-68
13. Duclos P, Redd SC, Varughese P, Hersh BS. Measles in adults in Canada and the United States: Implications for measles elimination and eradication. Int J Epidemiolo. 1999;28(1):141-146
14. Ong G, Hoon HB, Ong A, Chua LT, Kai CS, Tai GK. A 24-year review on the epidemiology and control of measles in Singapore, 1981-2004. S-E Asian J Trop Med Public Health. 2006;37(1):96-101
15. Thakur JS, Ratho RK, Bhatia SPS, Grover R, Issaivanan M, Ahmed B, Parmar V, Swami HM. Measles outbreak in a periurban area of Chandigarh: Need for improving vaccine coverage and strengthening surveillance. Ind J Pediatr. 2002;69(1):33-37
16. Chuang SK, Lau YL, Lim WL, Chow CB, Tsang T, Tse LY. Mass measles immunization campaign: Experience in the Hong Kong Special Administrative Region of China. Bull WHO. 2002;80(7):585-591
17. Cutts FT, Henderson RH, Clements CJ, Chen RT, Patriarca PA. Principles of measles control. Bull WHO. 1991;69(1):1-7
18. Borus PK, Cumberland P, Sonoiya S, Kombich J, Tukei PM, Cutts FT. Measles trends and vaccine effectiveness in Nairobi, Kenya. E Afr Med J. 2003;80(7):361-364
19. Kadri SM, Parray SH, Rubina S, Gaash BA, Danish M, Aesha F, Jan Y. Changing Face of Measles in Kashmir, India. Mid East J Family Med. 2008;6(9):19-22
20. Sniadack DH, Moscoso B, Aguilar R, Heath J, Bellini W, Chuy Chiu M. Measles epidemiology and outbreak response immunization in a rural community in Peru. Bull WHO. 1999;77(7):545-552
21. Pan Am Health Org. Measles eradication field guide; Technical paper no.41. Washington, DC: Pan Am Health Org. 1999:23-30
22. Abdool Karim SS, Abdool Karim Q, Chamane M. Impact of a measles immunization campaign on measles admissions to a Natal hospital. S Afr Med J. 1991;80:579-81
Author contact
![]() Corresponding author: Email: k-gotoac.jp
Corresponding author: Email: k-gotoac.jp

 Global reach, higher impact
Global reach, higher impact